Smartphone photogrammetry – affordable alternative for digitizing dental casts
Fotogrametria com smartphone – alternativa acessível para digitalizar modelos odontológicos
Fotogrametría con smartphone – alternativa accesible para digitalizar modelos odontológicos
DOI: 10.59681/2175-4411.v17.2025.1135
Wislem Miranda de Mello
Postgraduate Student, Postgraduate Program in Dental Sciences, Federal University of Santa Maria (UFSM), Santa Maria, Rio Grande do Sul, Brasil.
https://orcid.org/0000-0002-8594-7740
Vinícius Dutra
Clinical Associate Professor, Department of Oral Pathology, Medicine, and Radiology, Indiana University School of Dentistry (IUPUI), Indianapolis, Indiana, United States of America.
https://orcid.org/0000-0002-0534-3067
Magáli Beck Guimarães
Adjunct Professor, Department of Restorative Dentistry, Federal University of Santa Maria (UFSM), Santa Maria, Rio Grande do Sul, Brasil.
https://orcid.org/0000-0001-5130-7262
Jeannie M. Vickery
Clinical Associate Professor, Department of Prosthodontics, Indiana University School of Dentistry (IUPUI), Indianapolis, Indiana, United States of America.
https://orcid.org/0000-0001-5101-9017
Gabriela Salatino Liedke
Adjunct Professor, Department of Stomatology (UFSM), Federal University of Santa Maria (UFSM), Santa Maria, Rio Grande do Sul, Brasil.
https://orcid.org/0000-0002-0967-9617
Autor Correspondente: Wislem Miranda de Mello
Artigo recebido: 13/07/2024 | Aprovado: 26/05/2025
ABSTRACT
Objective: This article presents a simple and cost-effective protocol for digitizing dental casts using a smartphone and dedicated free software. Methods: A dental cast was digitized through photogrammetry using a smartphone and also with a laboratory scanner. The Root Mean Square (RMS) error was used to quantify the average deviation between the methods and to evaluate the accuracy of the digital models. Results: The comparison between the photogrammetry-generated cast and the same cast digitized with the laboratory scanner showed an RMS error ranging from 0.16 mm to 0.37 mm. The RMS error between three consecutive smartphone-based photogrammetry scans ranged from 0.16 mm to 0.35 mm. Conclusion: Smartphone-based photogrammetry enabled the digitization of the dental cast and its integration into the digital workflow for use in dental clinical planning.
Descriptors: Computer-Aided Design; Photogrammetry; Smartphone.
RESUMO
Objetivo: Este artigo apresenta um protocolo simples e econômico para digitalização de modelos odontológicos utilizando smartphone e software gratuito dedicado. Métodos: Um modelo odontológico foi digitalizado por fotogrametria utilizando um smartphone, e por um scanner de laboratório. A Média Quadrática (RMS) foi utilizada para quantificar o desvio médio entre os métodos e avaliar a acurácia dos modelos digitais. Resultados: A comparação entre o modelo gerado e o mesmo modelo digitalizado com scanner de laboratório mostrou RMS entre 0,16mm e 0,37mm. O RMS entre três fotogrametrias consecutivas do smartphone variou de 0,16mm a 0,35mm. Conclusão: A digitalização por smartphone permitiu a digitalização do modelo odontológico e sua inserção no fluxo de trabalho digital para utilização no planejamento clínico odontológico.
Descritores: Desenho Assistido por Computador; Fotogrametria; Smartphone.
RESUMEN
Objetivo: Este artículo presenta un protocolo simple y rentable para digitalizar modelos dentales utilizando un teléfono inteligente y un software gratuito dedicado. Métodos: Un modelo odontológico fue digitalizado mediante fotogrametría utilizando un smartphone, y mediante un escáner de laboratorio. La Media Cuadrática (RMS) se utilizó para cuantificar la desviación media entre los métodos y evaluar la precisión de los modelos digitales. Resultados: La comparación entre el modelo generado y el mismo modelo digitalizado con un escáner de laboratorio mostró una media cuadrática (RMS) entre 0,16 mm y 0,37 mm. El RMS entre tres fotogrametrías consecutivas de teléfonos inteligentes osciló entre 0,16 mm y 0,35 mm. Conclusión: El escaneo con teléfonos inteligentes permitió la digitalización del modelo dental y su inserción en el flujo de trabajo digital para su uso en la planificación dental clínica.
Descriptores: Diseño Asistido por Computadora; Fotogrametría; Teléfono Inteligente.
INTRODUCTION
Dentistry is in the era of the digital workflow. Diagnosis and treatment planning have significantly benefited from the use of computed tomography, computer-aided design and manufacturing (CAD-CAM) technology, augmented and virtual reality, and artificial intelligence (AI)(1,2). Models of the dental arches are highly useful in clinical dental practice, and to be integrated into the digital workflow, they need to undergo digitization of the dental casts using laboratory scanners or intraoral scanners(3,4). Both methods offer clinical accuracy and have inherent advantages and disadvantages; however, the cost of this equipment remains a barrier for most dental practices(3,4).
In this context, an alternative for dental cast digitization is photogrammetry. This technique involves capturing a series of standardized photographs to digitally reconstruct real objects or individuals using dedicated software(5–9). In dentistry, photogrammetry has been applied for facial scanning and for the digitization of scan bodies in virtual prosthetic planning(10,11). However, its potential for other applications, such as in forensic dentistry(12) and the digitization of dental models within the digital workflow, is still being explored. Previous studies have shown that the use of Digital Single-Lens Reflex (DSLR) cameras results in digital models without significant differences from the original dental casts, allowing for diagnosis and treatment planning in orthodontics, implantology, and restorative dentistry(5–7,9). Nevertheless, the use of DSLR cameras in dental offices remains expensive and limited. Smartphones are widely available nowadays, and recent improvements in smartphone camera quality may facilitate communication among healthcare professionals and enable the creation of high-quality 3D models. The smartphone has emerged as an interesting tool for clinical use(13–15).
Therefore, the objective of this article is to describe a cost-effective and straightforward protocol using the photogrammetry technique and a smartphone, aiming at its integration into the digital dental workflow.
METHODOLOGY
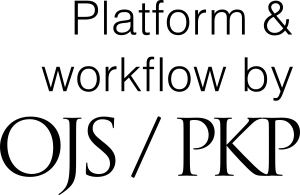
A dental plaster cast was obtained from a silicone impression of an upper arch mannequin, and randomly arranged lines were drawn over the areas of interest (teeth, gums, and mucosa) (Fig. 1).
Figure 1. Plaster model colored with red and black graphite; anterior (A) and posterior (B) views.
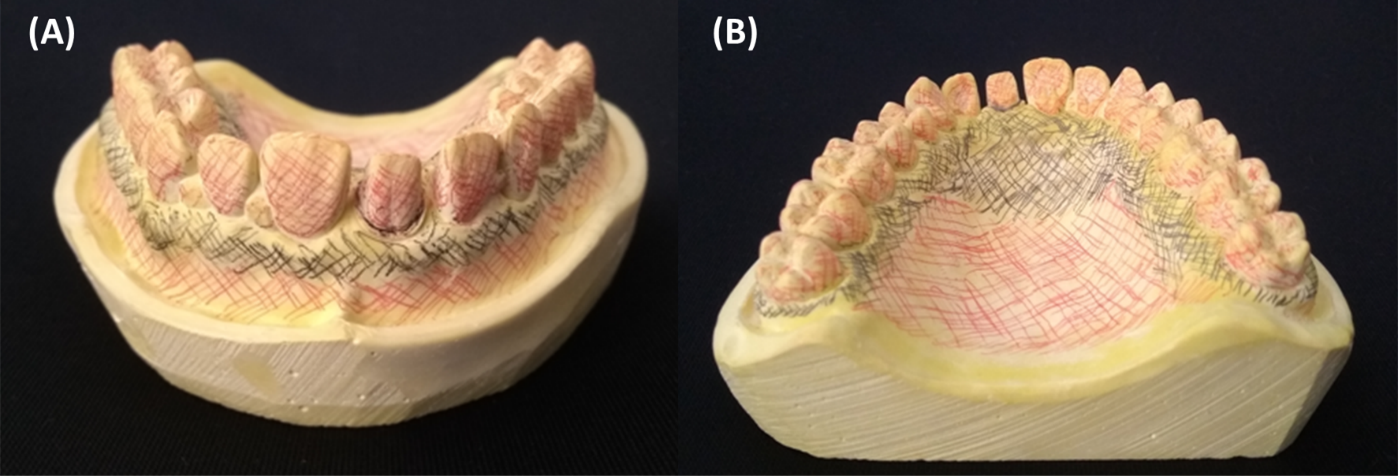
The photogrammetry method utilized a photographic guide (Fig. 2) to standardize the setup. The dental cast and a reference object with known dimensions were positioned centrally within the work area under ambient light conditions. Fifty photographs (taken from varying heights and angles) were captured using a smartphone (Motorola/Moto G5S Plus, 13MP Camera, f/2.0) mounted on a tripod for stabilization. The smartphone camera settings were adjusted to manual mode, with the following parameters: manual focus, ISO 100, ¼ shutter speed, and flash off. In the first step, 24 photographs were taken with the smartphone positioned at an angle of 60 degrees to the ground and a height of 20cm; these photos were captured at 15-degree intervals around the work area (depicted by black lines in Fig. 2 and 3A). In the second step, 24 photographs were taken with the smartphone positioned at an angle of 55 degrees to the ground and a height of 21 cm; again at 15-degree intervals (depicted by red lines in Fig. 2 and 3B). In the third step, 2 photographs were taken with the smartphone positioned at an angle of 45 degrees to the ground and a height of 23 cm; one photo was taken from an anterior perspective (position 1), and the other from a posterior perspective (position 25) relative to the setup (Fig. 2 and 3C).
Figure 2. Photographic guide displaying the work area and indicating the orientation of the smartphone camera and number of pictures for the photographic protocol.
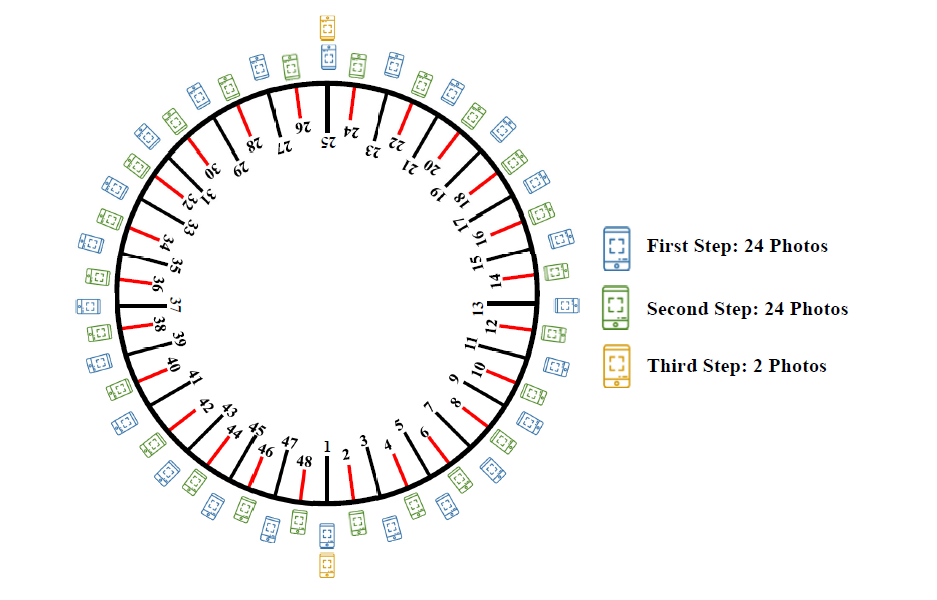
Figure 3. Three steps of the photographic protocol showing different heights and angles relative to the ground: first step (A), second step (B), and third step (C).
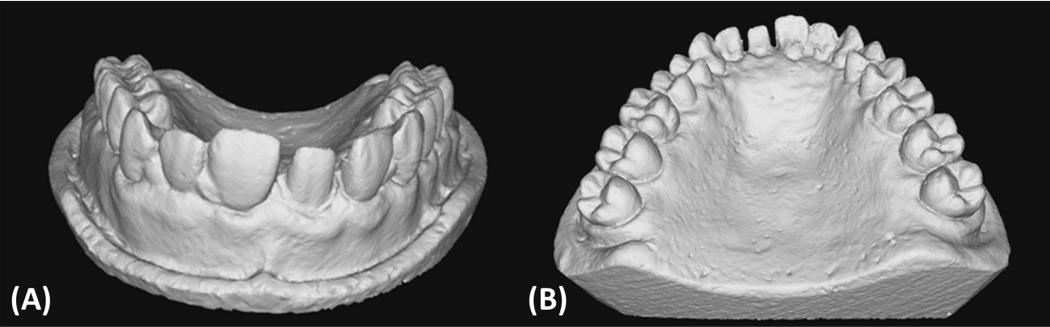
The 50 photographs were uploaded to a computer (Windows 10, Intel® CoreTM i5-4200U CPU @ 1.60GHz, Intel® HD Graphics Family, 8GB RAM) and imported into the photogrammetry software 3DF Zephyr Free (3D Flow, Verona, Italy). The digital model was generated using settings for camera orientation, dense point cloud creation, surface reconstruction, and texturing, all selected under the 'general' category with the highest quality presets. The digital model was resized to its real dimensions using a scale factor obtained from the ratio between the actual size of the reference object and its digital dimensions. Finally, the digital model was trimmed to the areas of interest using the software's editing tools and exported in .obj file format, including the 3D object textures (Fig. 4). The rendered object can also be visualized without textures (Fig. 5).
Figure 4. Digital model obtained after resizing, with the photographic background removed; anterior (A) and posterior (B) textured views.
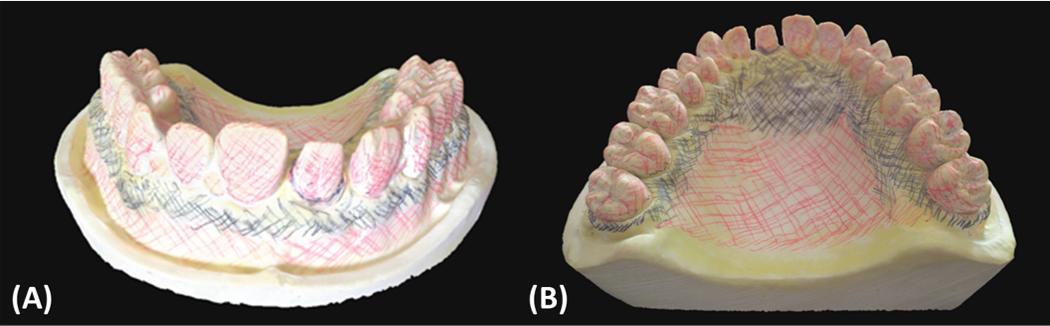
Figure 5. Digital model visualized without textures; anterior (A) and posterior (B) views.
The photogrammetry acquisition and digital model generation process were repeated three times. The study reference standard was the dental cast digitized with a laboratory scanner (E1; 3Shape, Copenhagen, Denmark). Geomagic Control X software (3D Systems, Rock Hill, USA) was used to compare the digital models in pairs and assess surface deviation. The accuracy of the photogrammetry method was evaluated using descriptive statistics: root mean square (RMS) and standard deviation (SD).
RESULTS AND DISCUSSION
The RSM quantifies the average deviation between the corresponding points on the surface of two models, providing a single numerical value that reflects both trueness and consistency. The RMS between the model digitized with a laboratory scanner and the digital models obtained with the photogrammetry method was 0.33 mm (SD 0.32) for the first smartphone photogrammetry (SP1), 0.16 mm (SD 0.16) for the second smartphone photogrammetry (SP2), and 0.37 mm (SD 0.36) for the third smartphone photogrammetry (SP3) (Fig. 6).
The discrepancy between the three consecutive acquisitions using the photogrammetry method showed an RMS of 0.29 mm (SD 0.28) for SP1 and SP2, 0.16 mm (SD 0.16) for SP1 and SP3, and 0.35 mm (SD 0.33) for SP2 and SP3 (Fig. 7). The highest discrepancies were observed on the proximal, palatal, buccal, and occlusal surfaces of the posterior teeth, suggesting the influence of shadows during image capture.
Figure 6. Superimposition between models scanned using the photogrammetry method and the laboratory scanner.
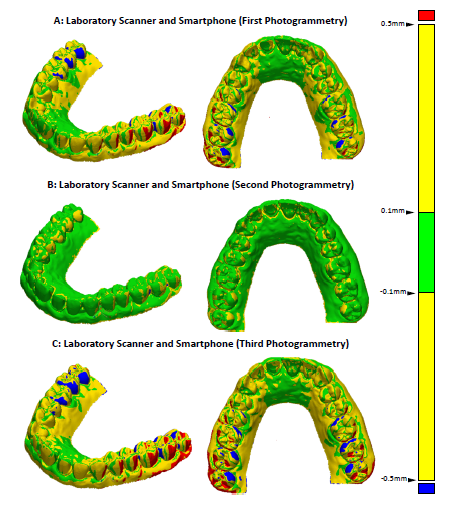
The color map on the right depicts the discrepancy: green, discrepancy up to 0.1 mm; yellow, discrepancy from 0.1 to 0.5 mm; red and blue, discrepancy greater than 0.5 mm.
Figure 7. Superimposition between three consecutive acquisitions using the photogrammetry method.
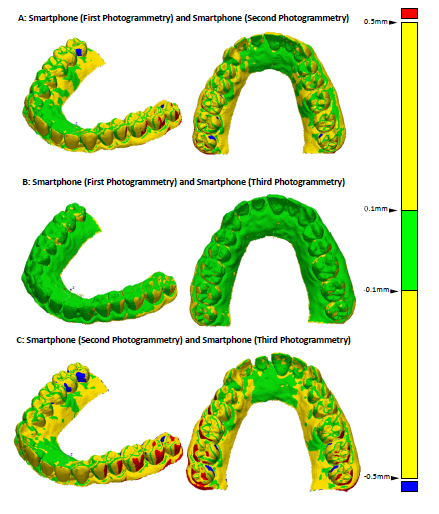
The color map on the right depicts the discrepancy: green, discrepancy up to 0.1 mm; yellow, discrepancy from 0.1 to 0.5 mm; red and blue, discrepancy greater than 0.5mm.
The use of digital data in dentistry represents a disruptive process. To support this new reality, the workflow presented in this article aims to make the photogrammetry technique more affordable and standardized while extracting the highest possible quality of digital reconstruction from the dental cast using a smartphone.
For result interpretation, the RMS value, along with the color map, provides a more reliable assessment when comparing two 3D models in Standard Triangle Language (STL) format. Unlike the mean, which may underestimate local surface discrepancies, the RMS accounts for both the magnitude and distribution of deviations across the entire surface. Therefore, RMS was chosen as the primary statistical measure to quantitatively evaluate the accuracy of the photogrammetry method in digital model comparisons(16,17). In this study, the RMS values between the models generated by photogrammetry and those obtained using a laboratory scanner ranged from 0.16 mm to 0.37 mm. Despite differences in visual appearance and mesh density, these values are considered acceptable for preliminary digital analysis, case planning, and dental cast digitization for database purposes.
Smartphone photogrammetry offers a low-cost alternative to laboratory scanners, with potential applications in both clinical and academic contexts. In dentistry, photogrammetry is already employed as a precise system for transferring implant positions by recording the spatial locations of components in the dental arch and integrating them into pre-existing 3D models(11). Other research groups have proposed using smartphone photogrammetry in fields such as forensic dentistry, maxillofacial prosthetic planning, and as a low-cost substitute for intraoral scanners in edentulous arch registration(12,18,19). Recent studies have reported linear discrepancies smaller than 0.5 mm when using smartphone photogrammetry for digitizing dental models, corroborating the findings of this research(20–22). However, the method may still fall short in highly sensitive applications, such as the manufacture of surgical guides or dental prostheses, considering that steps like 3D printing can further accentuate the differences between the printed object and the patients' dental arch(17). In this context, the present study contributes to broadening the use of photogrammetry and supports the inclusion of new users in the digital dental workflow. Future research should focus on optimizing image acquisition protocols, software parameters, and equipment configurations to establish accessible, reproducible, and high-quality photogrammetry workflows.
The smartphone has proven to be a valuable aid in various health-related tasks, including research in databases, use of health-related applications, visualization of digital images, and communication between professionals and patients(13,23,24). Nonetheless, despite its versatility, the smartphone still cannot replicate all the functionalities of dedicated equipment such as computers or photographic cameras. DSLR cameras are professional devices equipped with lenses that allow better control over the focal area, ensuring greater precision and quality in the captured images. Thus, certain adaptations or external equipment may be necessary when taking photographs with smartphones to improve image quality(12,14,20). Likewise, smartphones generally lack the processing power of computers, especially for rendering 3D images, as they do not contain high-performance graphics processing units (GPUs). At the time this study was conducted, mobile platforms offered limited options for 3D scanning applications, which is why the photogrammetry workflow described here relied on a laptop for image processing. More recently, however, a growing number of mobile applications have become available for 3D object scanning(8). Features such as augmented reality (AR) and cloud processing facilitate image acquisition and enable real-time 3D rendering directly on smartphones, which may increase the clinical adoption of this method. Furthermore, the integration of AI into these software solutions is expected to enhance the quality and accuracy of 3D reconstructions(10,25).
This study demonstrates promising results and practical applicability. Nonetheless, several methodological limitations should be acknowledged. The digitization process was performed by a single trained operator, and only one dental cast and one smartphone model were used, limiting the generalizability of the results to broader clinical and technical contexts. Moreover, smartphone-based photogrammetry involves a steep learning curve, which may influence outcome quality. The process appeared to be affected by factors such as the camera model, smartphone brand, photograph quality, ambient lighting conditions, object characteristics, and the operator’s experience. Future studies involving multiple operators, various smartphone models, a broader range of dental casts, and a larger number of acquisitions are recommended to further validate and extend these findings, ultimately supporting the integration of this technique into digital dental workflows.
CONCLUSION
The method presented in this study enabled accurate and reliable digitization of dental casts, demonstrating minimal discrepancies, making it suitable for study and planning in various clinical scenarios. Digitized models also offer greater security in the event of damage or loss of physical models and facilitate information sharing among interdisciplinary teams, as well as database storage for research purposes. Smartphone-based photogrammetry represents a viable and accessible alternative to laboratory scanners for dental cast digitization, making this technology available to all dental offices and universities.
ACKNOWLEDGMENTS
W. M. M. acknowledges the support of the Coordination for Funding and Support of Tertiary Education (CAPES), Brazil (grant No. 88887.721260/2022-00)
REFERENCES
1. Alauddin MS, Baharuddin AS, Mohd Ghazali MI. The Modern and Digital Transformation of Oral Health Care: A Mini Review. Healthcare. 2021; 9: 118.
2. Tallarico M. Computerization and Digital Workflow in Medicine: Focus on Digital Dentistry. Materials. 2020; 13: 2172.
3. Emir F, Ayyıldız S. Evaluation of the trueness and precision of eight extraoral laboratory scanners with a complete-arch model: a three-dimensional analysis. J Prosthodont Res. 2019; 63: 434-439.
4. Mangano F, Gandolfi A, Luongo G, et al. Intraoral scanners in dentistry: A review of the current literature. BMC Oral Health; 17. Epub ahead of print 2017. DOI: 10.1186/s12903-017-0442-x.
5. Fu X, Peng C, Li Z, et al. The application of multi-baseline digital close-range photogrammetry in three-dimensional imaging and measurement of dental casts. PLoS One; 12. Epub ahead of print 2017. DOI: 10.1371/journal.pone.0178858.
6. Stuani VT, Ferreira R, Manfredi GGP, et al. Photogrammetry as an alternative for acquiring digital dental models: A proof of concept. Med Hypotheses. 2019; 128: 43-49.
7. Zotti F, Rosolin L, Bersani M, et al. Digital Dental Models: Is Photogrammetry an Alternative to Dental Extraoral and Intraoral Scanners? Dent J (Basel). Epub ahead of print 2022. DOI: 10.3390/dj10020024.
8. Jindanil T, Xu L, Fontenele RC, et al. Smartphone applications for facial scanning: A technical and scoping review. Orthod Craniofac Res. 2024; 27: 65-87.
9. Chaudhary S, Kumar S, Aggarwal R, et al. Evaluation of the Accuracy of Digital Models Generated Using Photogrammetry. Cureus. Epub ahead of print 10 December 2024. DOI: 10.7759/cureus.75448.
10. Lee JD, Nguyen O, Lin Y-C, et al. Facial Scanners in Dentistry: An Overview. Prosthesis. 2022; 4: 664-678.
11. Hussein MO. Photogrammetry technology in implant dentistry: A systematic review. J Prosthet Dent. 2023; 130: 318-326.
12. Kurniawan A, Chusida A, Utomo H, et al. 3D Bitemark Analysis in Forensic Odontology Utilizing a Smartphone Camera and Open-Source Monoscopic Photogrammetry Surface Scanning. Pesqui Bras Odontopediatria Clin Integr; 23. Epub ahead of print 2023. DOI: 10.1590/pboci.2023.001.
13. Mosa ASM, Yoo I, Sheets L. A systematic review of healthcare applications for smartphones. BMC Medical Informatics and Decision Making; 12. Epub ahead of print 2012. DOI: 10.1186/1472-6947-12-67.
14. Hardan LS, Moussa C. Mobile dental photography: a simple technique for documentation and communication. Quintessence Int (Berl). 2020; 51: 510-518.
15. Teruya K, Park JH, Bay C. Dental photography using digital single-lens reflex cameras vs smartphones. AJO-DO Clinical Companion. 2025; 5: 26-34.
16. Emara A, Sharma N, Halbeisen FS, et al. Comparative evaluation of digitization of diagnostic dental cast (plaster) models using different scanning technologies. Dent J (Basel); 8. Epub ahead of print. 2020. DOI: 10.3390/DJ8030079.
17. Papaspyridakos P, Chen Y, Alshawaf B, et al. Digital workflow: In vitro accuracy of 3D printed casts generated from complete-arch digital implant scans. J Prosthet Dent. 2020; 124: 589-593.
18. Farook TH, Jamayet N bin, Asif JA, et al. Development and virtual validation of a novel digital workflow to rehabilitate palatal defects by using smartphone-integrated stereophotogrammetry (SPINS). Sci Rep; 11. Epub ahead of print. 2021. DOI: 10.1038/s41598-021-87240-9.
19. Saghiri MA, Saghiri AM, Samadi E, et al. Advancing 3D dental scanning: The use of photogrammetry with light detection and ranging for edentulous arches. J Prosthet Dent. Epub ahead of print December. 2024. DOI: 10.1016/j.prosdent.2024.10.032.
20. Jiang Y, Long H, Soo SY, et al. Accuracy of Complete-Arch Scans Obtained by Intraoral Scanner and Smartphone Three-Dimensional Scanning Applications with Different Smartphone Position Setups: An In Vitro Study. Cureus. Epub ahead of print 29 June 2024. DOI: 10.7759/cureus.63471.
21. Al-Rudainy D, Adel Al-Lami H, Yang L. Validity and reliability of three-dimensional modeling of orthodontic dental casts using smartphone-based photogrammetric technology. J World Fed Orthod. 2023; 12: 9-14.
22. Al-Tameemi R, Hamandi S, Al-Mahdi A. Creating a Digital 3D Model of the Dental Cast Using Structure-from-Motion Photogrammetry Technique. International Journal of Online and Biomedical Engineering (iJOE). 2023; 19: 4-17.
23. Schallenberger V, Maracci LM, Malta CP, et al. Smartphone Use for Tomographic Evaluation: Application in Endodontic Diagnosis. J Endod. Epub ahead of print 2022. DOI: 10.1016/j.joen.2022.01.017.
24. Pascadopoli M, Zampetti P, Nardi MG, et al. Smartphone Applications in Dentistry: A Scoping Review. Dent J (Basel). 2023; 11: 243.
25. Shilov L, Shanshin S, Romanov A, et al. Reconstruction of a 3D Human Foot Shape Model Based on a Video Stream Using Photogrammetry and Deep Neural Networks. Future Internet. 2021; 13: 315.